Sleep and Snoring
Sleep, Snoring and Obstructive Sleep Apnea (OSA)
The most important sleep condition to go undiagnosed and untreated is Obstructive Sleep Apnea (OSA), where recurrent airway collapse leads to frequent dips in oxygen levels. It is a serious condition because this chronic lack of oxygen supply to vital body organs such as the brain and heart may lead to heart failure, strokes, sudden death and even reduced life expectancy, if left untreated over time. It typically presents with loud snoring, daytime tiredness and fatigue, poor sleep quality and choking episodes when asleep. The patient usually does not notice these symptoms at first and more often, it tends to be detected by his sleep partner whose own sleep quality is disturbed in turn.
A good quality sleep study is important to aid diagnosis and management of OSA. The sleep study involves the patient sleeping according to his normal routine and pattern, whilst attached via several fine cables to a machine which will monitor his parameters during the night, such as oxygen saturation levels and heart rate. The sleep study can be arranged either at home or in hospital, depending on the patient’s clinical scenario, as some patients may require a much more detailed sleep study in hospital. However, most sleep studies are now usually undertaken at home, in the comfort of the patient’s own bedroom.

The sleep study is important as it is able to detect the number of episodes when the patient stops breathing (apnoea event) and when he does not breathe adequately (hypopnoea event). It also monitors the heart rate, breathing pattern, oxygen saturation, body position and other types of obstructive breathing episodes. This gives an accurate reflection of the severity of OSA, to help decide what sort of treatment plan is most suitable for the patient.
What treatment is best for me?
There are several treatment options available to treat snoring and OSA but every patient is different and the best way therefore is to carefully tailor the treatment to suit each patient, rather than adopt a one-size-fits-all approach.
My patient’s own experience is featured in this case study on obstructive sleep apnea.
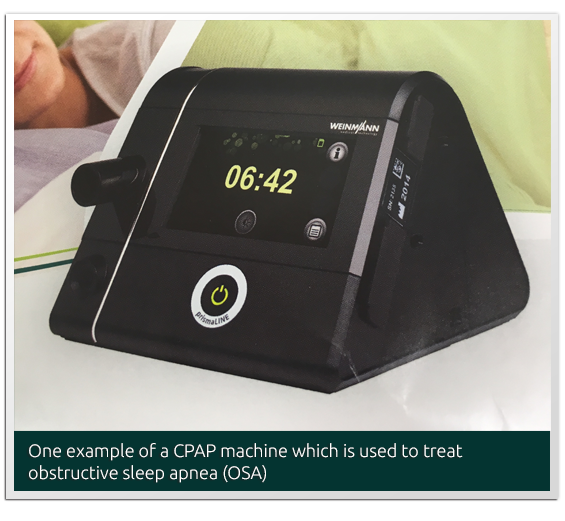
Continuous Positive Airway Pressure (CPAP) is the gold standard for OSA treatment. It is a special device used to keep the patient’s airways open by blowing in pressurised air to prevent the airways from collapsing shut. CPAP is delivered via a specially fitted mask over the nose and/or mouth to ensure a good seal of airflow coming from a small portable CPAP machine.
However, some patients may find CPAP uncomfortable or they just do not wish to wear a CPAP mask every night for the rest of their lives. Those who travel frequently may find it a hassle to bring along their CPAP wherever they go. In such patients, the option of surgery is a feasible one.
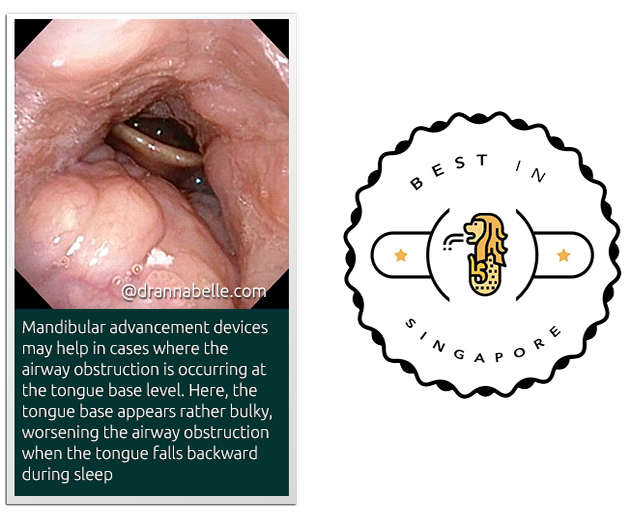
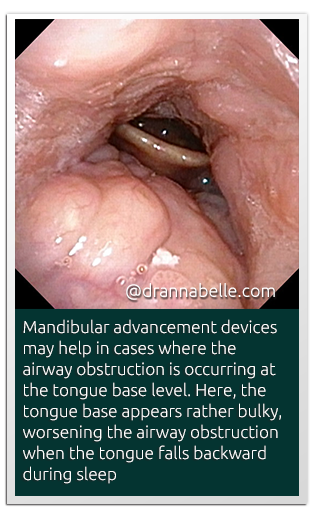
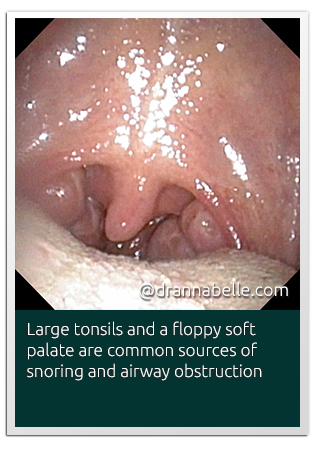
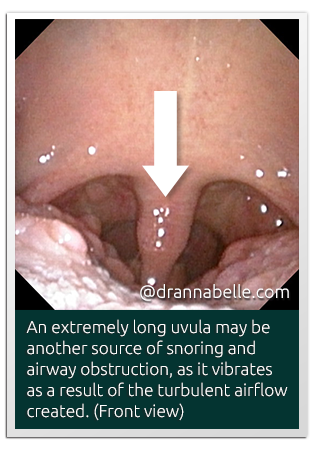
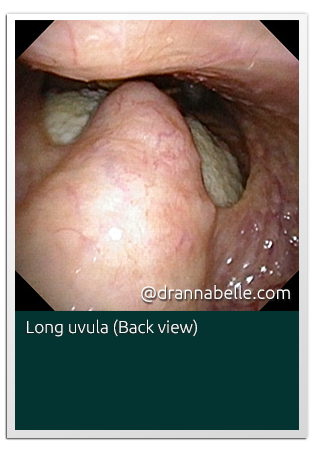
Surgery for OSA aims to remove any structural level of obstruction in the nose and throat to help the patient to breathe more clearly. Surgery may also have a supportive role to help the airflow delivery from the CPAP machine become much more efficient. Surgically correctable causes of obstruction in the nose and throat include enlarged nasal turbinates, deviated nasal septum, postnasal space mass or adenoid tissue, floppy redundant soft palate and uvula structures, as well as bulky tongue base tissue. The best patients for surgery tend to be those who are not obese and whose sleep study has not demonstrated severe OSA.
Mandibular Advancement Device
This special device looks like a retainer or mouthguard which is worn at night when the patient is asleep. It works best for patients whose jaw is on the smaller side or tends to fall backwards to block off the airway causing OSA.